As the final treatment for end-stage lung disease, lung transplantation can significantly extend patients’ survival time while substantially enhancing their quality of life. Over the past few decades, advancements in surgical techniques, immunosuppressive drugs, and post-transplant management have driven a surge in lung transplantation worldwide. From 2010 to 2018, nearly 34,000 lung transplants were performed worldwide. Lung transplant candidates and recipients constitute a unique group, primarily characterized by colonization and infections with multidrug-resistant (MDR) pathogens, recurrent lung infections, high biomass of the respiratory microbiota (particularly in the context of bronchiectatic lung disease), multiple microbial infections, reduced mucociliary clearance, and immunosuppression.
Globally, approximately 15%–20% of lung transplant recipients (LTRs) have underlying cystic fibrosis (CF), a distinct group characterized by younger patient age. In this group, multidrug-resistant pathogens cause a higher infection rate compared to other lung transplant recipients, along with a higher incidence of antibiotic allergies and an increased risk of infectious complications post-transplantation.

A recent study reported a marked increase in the number of lung transplants performed to treat COVID-19-related acute respiratory distress syndrome (ARDS) during the 2019 novel coronavirus (COVID-19) pandemic, with a notable rise from 2020 to 2022. In the United States, 8.7% of lung transplants during this period addressed COVID-19-related ARDS. Many patients require prolonged mechanical ventilation and extracorporeal membrane oxygenation (ECMO) prior to transplantation, which heightens their risk of nosocomial infections, particularly those caused by multidrug-resistant Gram-negative pathogens such as Pseudomonas aeruginosa, carbapenem-resistant Acinetobacter baumannii, and Aspergillus spp. Lung transplantation is contraindicated for patients with uncontrolled pulmonary or extrapulmonary infections; thus, lung transplant candidates must resolve their infections prior to receiving a transplant.
Infectious complications are the primary cause of mortality among lung transplant recipients, accounting for approximately 30% of deaths in the first year post-transplantation and about 20% in subsequent years. Common pathogens in the lung transplant context include Pseudomonas aeruginosa, methicillin-resistant Staphylococcus aureus, Burkholderia cepacia, Mycobacterium abscessus, Stenotrophomonas maltophilia, and Achromobacter xylosoxidans. These microorganisms are often multidrug-resistant, leaving patients with very limited treatment options.
01
Clinical Application of Bacteriophages in Lung Transplantation
Bacteriophage therapy has been employed in some lung transplant candidates and recipients, primarily targeting multidrug-resistant Gram-negative bacterial infections and atypical mycobacterial infections. Table 1 summarizes published treatment cases, including 11 lung transplant recipients and 2 lung transplant candidates, categorized by pathogen type, infection type, administration method, and clinical outcome. Overall, bacteriophage therapy was well tolerated, and most patients achieved successful outcomes. In 7 of the treated cases, the infection resolved clinically; four patients showed clinical improvement (though 2 of these patients died of non-infection-related causes during bacteriophage therapy, precluding assessment of the true outcome).

Table 1 Summary of Bacteriophage Therapy Cases Involving Lung Transplant Recipients and Candidates in Published Studies
Note: Clinical resolution refers to the resolution of symptoms at the end of treatment and a negative culture for the target pathogen; clinical improvement indicates symptom improvement but persistence or recurrence with a positive target bacteria culture; clinical failure includes lack of symptom improvement and persistent culture positivity.
02 Biodistribution of Bacteriophages In Vivo
In a 2019 report by Aslam et al., bacteriophage therapy was administered to three lung transplant recipients (LTRs) with multidrug-resistant bacterial infections caused by Pseudomonas aeruginosa (patients 1 and 2) and Burkholderia (patient 3) [4]. Researchers simultaneously assessed the specific biodistribution of bacteriophages in the respiratory tract of these patients during bacteriophage therapy.
Patient 1 received two consecutive weeks of intravenous infusion (days 1–15) and nebulization (days 16–29), both utilizing the bacteriophage cocktail AB-PA01, which, in its initial phase, comprises four strains of Pseudomonas aeruginosa phages. As depicted in Figure 1, no bacteriophages were detected in the alveolar lavage fluid prior to initiating bacteriophage therapy (Day 1). Bacteriophage detection reached approximately 4 × 10^7 PFU/ml in lavage samples collected 3 days (Day 4) after initiating intravenous AB-PA01 treatment and on Day 29 (when the patient received only nebulized AB-PA01 during the preceding week) (Figure 1). These findings indicate that both intravenously and aerosolized inhaled bacteriophages reach the lungs.
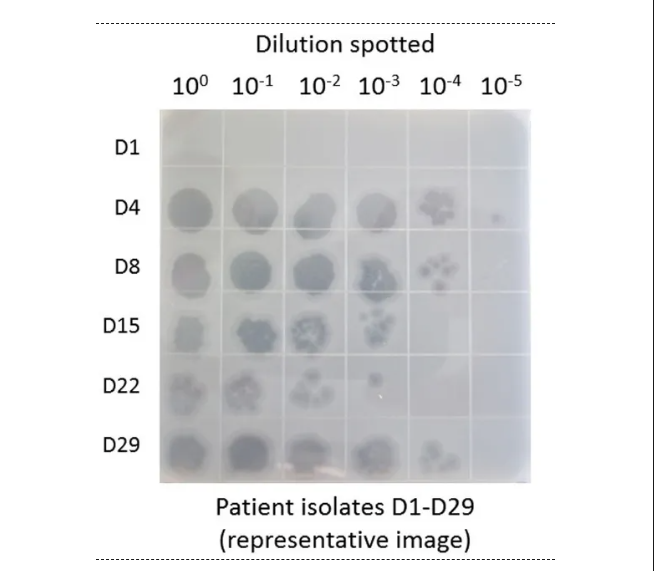
Figure 1 Detection Results of Active Bacteriophages in Alveolar Lavage Fluid During Treatment of Patient 1 with Cocktail AB-PA01 [1].
03 Safety Monitoring of Bacteriophage Therapy
A 2022 systematic review of approximately 270 patients found that bacteriophage therapy is generally quite safe, with an adverse event rate of 7%. Generally, it is recommended to monitor baseline and weekly complete blood counts, renal and liver function test results, and inflammatory markers in patients undergoing bacteriophage therapy. Since bacteriophages are highly specific to their bacterial hosts, there is a theoretical risk that targeted elimination of specific bacteria in the respiratory microbiome could allow other potentially more pathogenic microorganisms to occupy this ecological niche, potentially leading to clinical deterioration. Therefore, close monitoring of vital capacity and forced expiratory volume in one second (FEV1.0) is also recommended for lung transplant candidates and recipients.
As with any new therapeutic agent, anaphylactic reactions can occur with bacteriophage therapy, particularly related to excipients in the final product. In the United States, the Food and Drug Administration recommends close monitoring within 3 hours of the first dose of bacteriophage therapy. Professor Saima Aslam from the University of California, San Diego, stated that at their clinic, the Center for Innovative Bacteriophage Applications and Treatments, an anaphylaxis kit is placed at the patient’s bedside when the first dose of bacteriophage therapy is administered. The kit includes antihistamines, epinephrine injections, H2 blockers, nebulized salbutamol, and steroids (both oral and injectable).
04
The Latest Clinical Trial Research in the Field of Lung Diseases
04
As indicated in Table 2, several early-phase clinical trials are currently focusing on patients with cystic fibrosis, including one trial on cystic fibrosis bronchiectasis that enrolled patients with Pseudomonas aeruginosa colonization (Table 2). Additionally, an ongoing international registry for patients with cystic fibrosis (CF) and lung transplant recipients (LTRs) with complex Burkholderia colonization has been established and is currently operational in the United States. This registry collects bacterial isolates from enrolled patients, which have been used to develop a lytic bacteriophage library for preliminary clinical trials.
The aforementioned clinical trials evaluate the effectiveness of bacteriophage therapy by monitoring various endpoint metrics to assess its efficacy. These metrics include reductions in sputum microbiota, changes in lung function (evaluated by forced expiratory volume in 1 second), alterations in the airway microbiome composition, and clinical outcomes (such as changes in symptoms and hospitalization rates), alongside close monitoring of adverse events. Simultaneously, these trials also assess bacteriophage dynamics and pharmacodynamics, as well as the development of resistance and serum neutralization.

Table 2 Ongoing Clinical Trials Evaluating the Role of Bacteriophage Therapy in Lung Diseases
Summary
Lung transplant candidates and recipients are burdened by diseases caused by multidrug-resistant pathogens, including Pseudomonas aeruginosa, Achromobacter xylosoxidans, Mycobacterium abscessus, and Burkholderia cepacia, among others, and are particularly vulnerable to infections by these pathogens. These pathogens not only directly cause disease and death but also impact treatment courses and post-transplant outcomes, including the development of chronic lung allograft dysfunction (CLAD). Bacteriophages, as a novel and highly targeted tool, can be applied in lung transplantation contexts in various ways, thereby influencing all these outcomes.
References
1.Chambers DC, Perch M, Zuckermann A, et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: thirty-eighth adult lung transplantation report—2021; focus on recipient characteristics. J Heart Lung Transplant 2021; 40:1060–72.
2.Okumura K, Jyothula S, Kaleekal T, Dhand A. 1-year outcomes of lung transplantation for coronavirus disease 2019–associated end-stage lung disease in the United States. Clin Infect Dis 2023; 76:2140–7.
3.Saima Aslam. Phage Therapy in Lung Transplantation: Current Status and Future Possibilities. Clin Infect Dis 2023 Nov 2;77(Supplement_5):S416-S422.
4.Aslam S, Courtwright AM, Koval C, et al. Early clinical experience of bacteriophage therapy in 3 lung transplant recipients. Am J Transplant 2019; 19:2631–9.
5.Uyttebroek S, Chen B, Onsea J, et al. Safety and efficacy of phage therapy in difficult-to-treat infections: a systematic review. Lancet Infect Dis 2022; 22: e208-20.



