Living-Related Kidney Transplantation

Introduction to Living-Related Kidney Transplantation
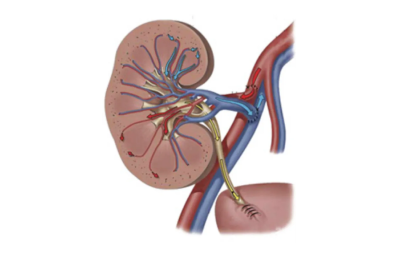
Overview
Living-related kidney transplantation is a surgical procedure in which a kidney is removed from a healthy relative and transplanted into a patient with uremia. Due to the severe shortage of donor kidneys, living-related kidney transplantation has become an important source of kidneys and a crucial supplement to deceased organ donation. This helps to alleviate the growing demand for kidney transplants and the shortage of donor kidneys.
Requirements for Family Relationships
In living-related kidney transplantation, the recipient and donor are typically required to have a certain familial relationship, such as parents, children, and spouses. For specific familial relationships, please click here. The closeness of these relationships helps increase the success rate of tissue matching and reduces the risk of immune rejection.
Preoperative Evaluation
Before the kidney transplant surgery, both the donor and the recipient need to undergo comprehensive and detailed medical evaluations to ensure the safety and success of the surgery. Preoperative tests include blood type matching, tissue matching, health assessments, and psychological evaluations.

Postoperative Management
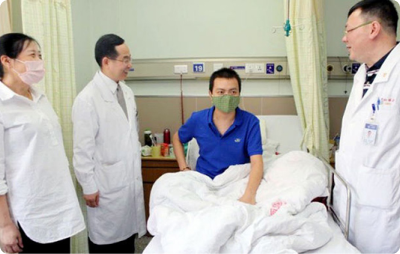
Postoperative management is crucial for the long-term survival of the transplanted kidney and the patient. Recipients need to undergo regular medical check-ups to monitor kidney function and the concentration and effectiveness of immunosuppressive drugs. Additionally, maintaining a healthy lifestyle, including taking medications on time, having a balanced diet, engaging in moderate exercise, and avoiding infections, is essential.
Quality of Life
Living-related kidney transplantation can significantly improve the quality of life for patients. A successful kidney transplant can restore normal kidney function, allowing them to return to daily activities and work. Moreover, donors can also quickly recover their health and continue to live a normal life after the surgery.
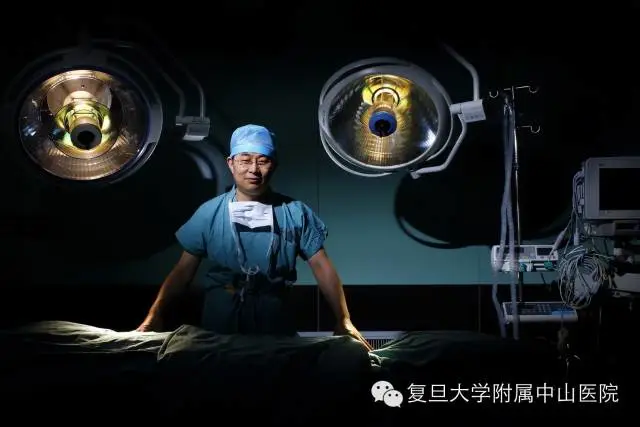
Living-related kidney transplantation is an effective and safe method of kidney transplantation, bringing new hope to many patients with kidney failure. The Kidney Transplant Department of Zhongshan Hospital, Fudan University, as one of the earliest units in China to conduct living-related kidney transplantation, is committed to providing the highest quality medical services to help patients regain their health.
Related Articles
Living-Related Kidney Transplantation: A Relay of Life
FAQs on Legal Regulations of Living-Related Kidney Transplantation
How Close Must the Family Relationship Be for Living-Related Kidney Transplantation?
Where Will My New Kidney Be Placed?
During Living Donor Nephrectomy – How Do We Protect the Donor?
Embracing New Life: Exploring the Recovery Miracles After Living-Related Kidney Transplantation
Advantages of Living-Related Kidney Transplantation
Living-related kidney transplantation offers several significant advantages.
Genetic Matching
In living-related kidney transplantation, the human leukocyte antigen (HLA) compatibility between the donor and recipient is often higher. This genetic matching helps reduce the risk of rejection of the new kidney by the recipient’s body. Due to the genetic similarity between relatives, the transplanted kidney is more likely to be accepted by the recipient’s body, improving the success rate and long-term survival of the transplant.
Higher Quality of Donor Kidneys
The quality of the donor kidney largely depends on the duration of warm and cold ischemia. Living-related kidney transplantation significantly reduces warm and cold ischemia times compared to DCD (Donation after Circulatory Death) kidneys. This minimizes ischemia-reperfusion injury, ensuring better kidney quality and faster, better recovery of kidney function after surgery.
Strong Emotional Connection
The coordination and communication between relatives are closer, which helps ensure the thorough implementation of preoperative preparations. The emotional support and connection between relatives have a positive impact on the recipient’s recovery and mental well-being.
Reduced Time and Economic Costs
Living-related kidney transplantation significantly shortens the waiting time for patients. Compared to DCD kidneys, living-related transplantation can be performed promptly once both the donor and recipient are ready. This avoids long waiting periods and associated health risks, accelerates the treatment process, and improves the quality of life. Additionally, living-related kidney transplantation reduces the economic burden on patients. The incidence of rejection is lower after living-related transplantation, and the dosage of immunosuppressive drugs required postoperatively is relatively lower.
Higher Safety for Donors
In recent years, the perioperative mortality rate for living kidney donors has dropped to a very low level. The glomerular filtration rate (GFR) of donors is approximately 65-70% of the preoperative level in the short term. In the long term, the mortality rate of living kidney donors is not significantly different from that of the general population. Recent studies have even shown that the mortality rate from cardiovascular causes is lower among living kidney donors than in the general population. Therefore, living-related kidney transplantation is safe for eligible donors, and their kidney function remains stable after surgery if they follow medical advice.
Related Articles
Living-Related Kidney Transplantation: When Family Members Become Superheroes
Living-Related Kidney Transplantation: A Gift of Life
Is It Safe to Donate a Kidney in Living-Related Transplantation?
Clinical Advantages of Living-Related Kidney Transplantation
Risks and Challenges of Living-Related Kidney Transplantation
Living-related kidney transplantation also involves some potential risks and challenges. The Kidney Transplant Department of Zhongshan Hospital, Fudan University, is committed to helping patients overcome these challenges and ensuring the health and safety of both donors and recipients.
Risks and Challenges for Donors
Surgical Risks
During kidney removal surgery, donors may face risks such as infection, bleeding, and organ injury, although these are usually well-controlled.
Postoperative Complications
After donating a kidney, the remaining kidney must take on the full function. Donors may experience complications such as hypertension and reduced kidney function.
Psychological Burden
Donating a kidney is a significant decision, and donors may face psychological stress due to concerns about their postoperative health.
Metabolic Disease Risks
Donors may have an increased risk of developing metabolic diseases (such as diabetes and hyperlipidemia) after donation. Long-term health monitoring and lifestyle management are crucial.
Risks and Challenges for Recipients
Risk of Rejection
Even with genetic similarities between relatives, recipients still need to take immunosuppressive drugs long-term to prevent their immune system from attacking the transplanted kidney.
Side Effects of Immunosuppressive Drugs
Long-term use of immunosuppressive drugs can increase the risk of infections, tumors, diabetes, and other metabolic diseases.
Postoperative Complications
Recipients may experience complications such as hypertension and diabetes after surgery, and chronic damage to the transplanted kidney (such as interstitial fibrosis and tubular atrophy) may occur.
Medication Adherence Issues
Recipients need to take multiple immunosuppressive drugs long-term, but some may fail to strictly follow the medication regimen due to side effects, cost, or other reasons. This increases the risk of rejection and other complications.
Psychological Burden
The recovery process can be psychologically challenging for recipients, who may worry about the survival of the transplanted kidney and the quality of their postoperative life.
To address these potential risks and challenges, the Kidney Transplant Department of Zhongshan Hospital, Fudan University, conducts detailed preoperative assessments for both donors and recipients, uses advanced surgical techniques to minimize trauma, and ensures smooth surgery. Postoperatively, our medical team (doctors, nurses, and pharmacists) closely monitors both donors and recipients to handle any issues promptly. Additionally, the kidney transplant team combines artificial intelligence to provide lifelong health management for recipients. We will accompany both donors and recipients throughout the process, ensuring their health and quality of life through comprehensive medical management and psychological support.
Related Articles
The Bright Future of Living-Related Kidney Transplantation: Exploration and Outlook
Classic case
Love will have a miracle: successful wife cross -blooded wife donate kidneys for her husband
Incompatible blood type kidney transplantation
Classic case
Kidney transplant team
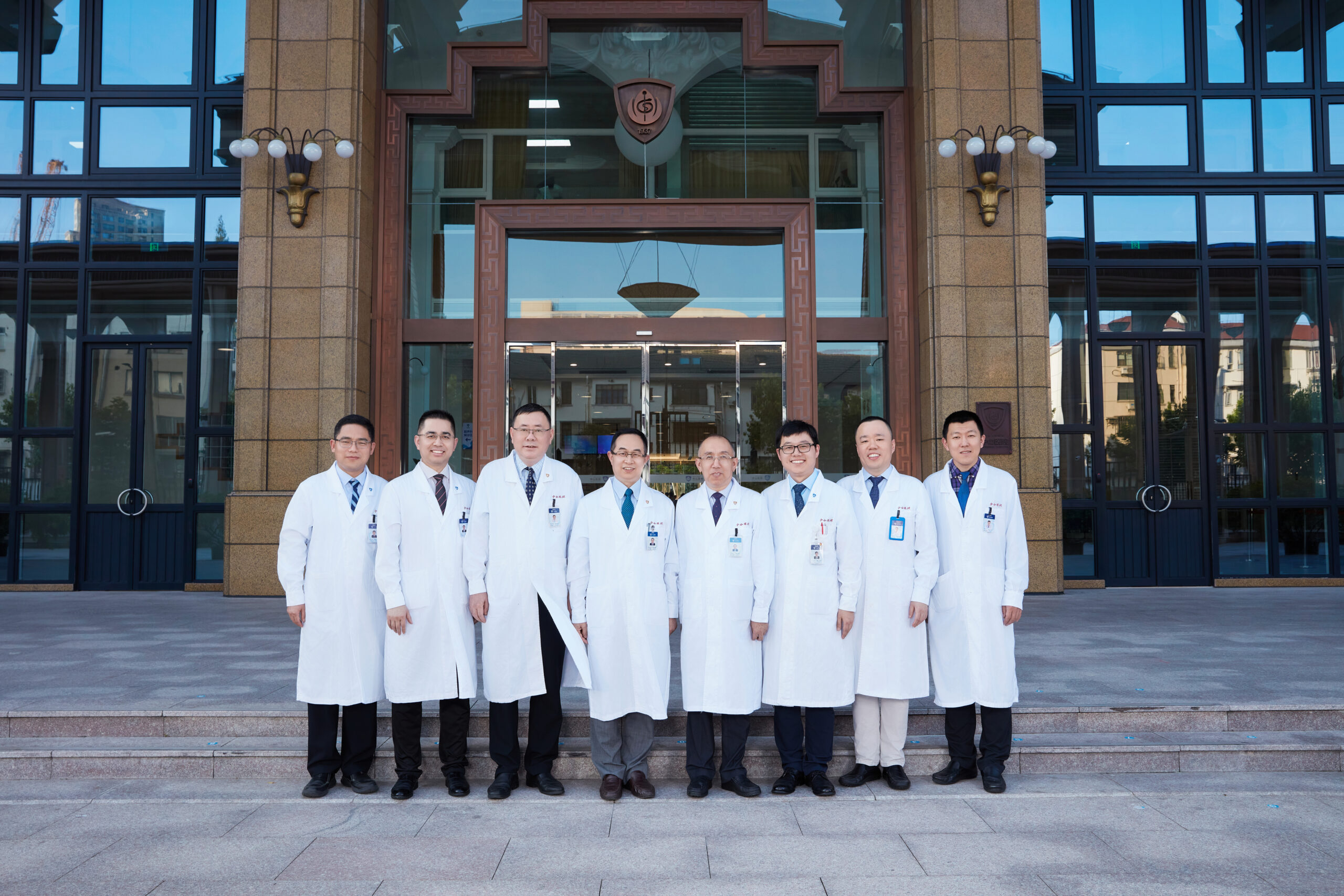
Professor Zhu Tongyu
MD, Chief Physician, PhD Supervisor
Professor Rong Ruiming
MD, Senior Professor of Surgery at Fudan University, PhD Supervisor

Professor Xu Ming
MD, Professor, Master’s Thesis Supervisor
Associate Chief Physician Wang Jinan
MD, Associate Chief Physician, Master’s Thesis Supervisor

Associate Chief Physician Yang Cheng
MD, Associate Chief Physician, Researcher (dual appointment), Master’s Thesis Supervisor
Associate Chief Physician Wang Xuanchuan
Doctor of Medicine (MD)
Attending Physician Qi Guisheng
Doctor of Medicine (MD)
Attending Physician Zhu Dong
Doctor of Medicine (MD)

Resident Physician Zhang Weitao
Doctor of Medicine (MD), Jointly Cultivated PhD: Fudan University and Harvard Medical School
Classic case
Procedure
Live-Related Kidney Transplantation Procedure
Due to the unique nature of live-related kidney transplantation (hereinafter referred to as “living donor kidney transplantation”), it is essential to ensure that the living donor is healthy and that the recipient does not have any contraindications for kidney transplantation. Therefore, preoperative examinations and assessments must be comprehensive and meticulous.
(I) Donor Evaluation
The health of the donor is paramount. Protecting the donor is the fundamental ethical principle of living donor kidney transplantation, and the donor’s well-being takes precedence over that of the recipient. A comprehensive health assessment of the donor is necessary. If significant health issues are identified, the individual is not suitable to be a donor. Given the extensive list of preoperative examinations, tests should be conducted in a stepwise manner, starting with simpler and less expensive procedures. If health issues are detected in the initial stages, further testing will not be pursued.
⑴ Initial Screening
Blood type, complete blood count (CBC), liver and kidney function, electrolytes, ion concentration, lipid profile, fasting blood glucose, and urinalysis (if proteinuria is detected, a 24-hour urine protein quantification should be added).
Ultrasound: thyroid, liver, gallbladder, pancreas, spleen, kidneys + ureters, bladder, adrenal glands, retroperitoneum, prostate and scrotal contents for males, and breast, uterus, and adnexa for females.
⑶ Final Examinations
HLA typing, radionuclide renal scan, kidney vascular CT (CTA, CTV).
(II) Recipient Evaluation
Recipients of kidney transplantation must undergo a comprehensive medical assessment to exclude contraindications for kidney transplantation. The evaluation process for recipients of living-related kidneys is similar to that for deceased donor (DCD) kidneys. The assessment items for kidney transplant recipients are as follows:
Routine Laboratory Tests
CBC, liver and kidney function, electrolytes, ion concentration, fasting blood glucose, lipid profile, blood typing (once at our hospital and once at an external hospital), complete coagulation profile, pre-transfusion panel, ESR, T-spot, PTH, lymphocyte typing, cytokines.
Virology-Related Tests
HBV DNA (for hepatitis B patients), HCV RNA (for hepatitis C patients), CMV antibody, rubella virus antibody, Toxoplasma antibody, EB virus antibody, BK virus nucleic acid quantification (blood and urine).
Tumor-Related Tests
PSA + fPSA (for males ≥50 years old), AFP, CEA, CA199, CA724, NSE, CA125, CA153 (for females), cervical cytology test (TCT for females ≥40 years old).
Imaging Studies
ECG, non-contrast chest CT, ultrasound (thyroid, liver, gallbladder, pancreas, spleen, kidneys, ureters, adrenal glands, retroperitoneum, breast and gynecological organs for females, scrotal contents and prostate for males), vascular ultrasound (iliac artery and vein), echocardiogram.
Tissue Typing Tests
HLA typing, panel reactive antibody (PRA), lymphocytotoxicity test.
After the above examinations and evaluations, if the kidney supply is healthy, and the recipient does not have the contraindications of kidney transplant surgery, you can enter the second stage of preparation before the relative kidney transplantation, that is, the ethical preparation and review stage.
(III) Ethical Preparation
Living donor kidney transplantation requires strict ethical approval. According to China’s “Regulations on Human Organ Transplantation,” living organ donors must be citizens aged 18 years or older; recipients of living organs are limited to the donor’s spouse, direct blood relatives, or collateral blood relatives within three generations.
The Department of Kidney Transplantation at Zhongshan Hospital, Fudan University, requires the following ethical materials and approval process for living donor kidney transplantation:
Identity Card Copies
Copies of the identity cards of the donor (donor), donor’s father and mother (biological parents), donor’s spouse, and donor’s children (hereinafter referred to as “donor and related parties”). Identity card copies are not required for minor children of the donor.
Copies of the recipient’s identity card (both sides). If the identity card is lost, a population information certificate must be issued by the local public security authority.
Proof of Relationship
Copies of the household registration books of the donor and related parties and the recipient, including the front page of the household registration book.
Household Registration Certificates and Requirements for Donor and Related Parties and Recipient
Must be issued by the local public security authority; relationship certificates issued by neighborhood committees or village committees are not accepted.
The household registration certificate must include the name and ID number of the person being certified.
The certificate must state the relationship between the donor and the recipient, the parent-child relationship between the donor and their parents, the marital relationship between the donor and their spouse, and the parent-child relationship between the donor and their children.
The certificate must be printed or photocopied, not handwritten, and must bear the official seal of the local public security authority (police station). The heading should原则上 be “Household Registration Certificate” (though it may vary according to local police station regulations), and it must include the signature of the handling officer, contact phone number, and date. The health commission will contact the officer to verify the authenticity of the certificate.
If the donor’s parents are deceased, a death certificate can be issued by the neighborhood committee or village committee, stating the relationship between the donor (name and ID number) and their parents (names), as well as the time of death, and bearing the committee’s seal. The death certificate may be handwritten.
For spousal kidney donation, a copy of the marriage certificate is required.
If the donor and related parties are in the same household registration book (and the donor and recipient are not separated), the household registration book can be photocopied, stamped by the police station, signed by the officer, and the phone number left. For related parties not in the same household registration book, the household registration certificate must be issued according to the above requirements 3 and 4.
Two-inch Individual Photos
One 2-inch individual photo for both the donor and the recipient.
Blood Type and Tissue Typing Reports
Blood type reports for both the donor and recipient from the Blood Transfusion Department of Zhongshan Hospital.
HLA, PRA, and CDC reports issued by the tissue typing laboratory of Zhongshan Hospital.
Required Examination Reports for Donor and Recipient
Donor: CBC, urinalysis, liver and kidney function, coagulation profile, fasting blood glucose, lipid profile, hepatitis B surface antigen and e antigen, hepatitis C antibody, HIV antibody, RPR, ECG, chest X-ray, abdominal ultrasound, CTA, ECT, and height and weight.
Recipient: recent CBC, liver and kidney function, coagulation profile, hepatitis B surface antigen and e antigen, hepatitis C antibody, HIV antibody, RPR reports.
After preparing all the required materials, the donor and recipient should bring the above documents, as well as the original identity cards, household registration books, and marriage certificate (for spousal donation) of all related parties, to Room 709, 7th Floor, Building 1, Zhongshan Hospital, Fudan University, every Tuesday from 2:00 PM to complete the procedures.
Upon verification of the materials, the following steps must be completed: signing the intention letter and informed consent form, and electronic chip verification of the original identity cards of the donor, related parties, and recipient.
After completing these steps, all materials will be submitted to the Zhongshan Hospital Ethics Committee for review. The committee will hold regular meetings to examine the cases. The donor, related parties, and recipient will be interviewed. Subsequently, the hospital will submit all materials to the Shanghai Municipal Health Commission’s Medical Management Department for further review. Upon approval, the department will send the approval letter back to our hospital, and the donor and recipient will wait for the notification to be admitted for surgery.
Note: The above items may vary based on the patient’s medical history.